90Yr Male with Altered sensorium
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
This is a case of 90 year old male came with complaints of
c/o cough since 15 days
SOB since 1 week
Loss of appetite since 1 week
Altered sensorium since 3 days
HOPI:
Patient was apparently asymptomatic 15 days ago then he developed cough insidious onset initially dry later productive and scanty.white to yellow not blood stained more during night. SOB since 1 week insidious onset gradually progessive ,progressed to grade 4, no orthopnea, No PND.No h/o seasonal/diurnal variation.
Loss of appetite since 1 week. No h/o fever, vomiting,pain abdomen,loose stools,giddiness. Altered sensorium since 3 days.
No relevant history in the past
Personal history:
Diet: mixed
Appetite: normal
Sleep: Adequate
Bowel and bladder: increased micturition(since 1week), normal bowel movements
No addictions and allergies
GENERAL EXAMINATION:
Vitals:
BP 120/70 MMHG
PR 92 BPM
RR 28/MIN
GRBS 93 MG/DL
SpO2 100% ON 6L O2
No pallor,No icterus, cyanosis, clubbing, lymphadenopathy.
SYSTEMIC EXAMINATION ::
GIT
INSPECTION :
Abdomen - scaphoid
Umbilicus - inverted
Movements - all quadrants are equally moving with respiration
No scars and sinuses
No visible peristalsis
No engorged veins.
PALPATION:
No local rise in temperature and no tenderness in all quadrants
LIVER: no hepatomegly
SPLEEN- not enlarged
KIDNEYS - bimanual palpable kidneys
PERCUSSION :
no shifting dullness
AUSCULTATION :
Bowel sounds are heard and are normal
No bruit
Respiratory system:
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
No tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- absent.
Vocal fremitus- normal on both sides.
Percussion:
Supraclavicular
Infraclavicular.
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Interscapular
Right side and left side- resonant in above areas.
Auscultation:
Bilateral Airway entry - present.
Decreased BS on the left side.
B/L crepts present in basal areas,wheeze present.
Cardiovascular system:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
Central Nervous system:
Higher motor functions- cannot be elicited
Speech: Normal
Cranial nerve functions - cannot be elicited
Sensory system- cannot be elicited
Motor system Right Left
Power- UL 4/5 4/5
LL 4/5 4/5
Neck Normal
Trunk muscles Normal
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps + +
Triceps + +
Supinator + +
Knee + +
Ankle + +
INVESTIGATIONS:
29/4/23
2/5/23
DIAGNOSIS :
Altered sensorium secondary to ? TB meningitis ? pyogenic meningitis
?AKI ( Pre renal) resolved
?COPD(emphysematous)
? B/L pulmonary koch's with iron deficiency Anemia
TREATMENT:
1. IV FLUIDS NS @ 75 ml/hr
2. RT feed
200 ml water 2 nd hrly
200 ml milk 4th hrly
3. Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
Mucomist - 4 th hrly
4.SYP.GRILLINCTUS - 15 ml RT/TID
5.CPAP - Intermittently
6.Oxygen support to maintain spo2 88-94%
7.GRBS - 7 POINT PROFILE
8.Vitals monitoring 2nd hrly.
Follow up
30/4/23
S
Stools passed
No fever
O
Pt is conscious, coherent and irritable
Speech is normal
No meningeal signs
GCS E 4 V4 M5
BP - 130/80 mm hg
PR - 92 bpm
SPO2: 96% ON 6L O2
RR: 28 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , B/L CREPTS + ,WHEEZE +
CNS: E4V4M5
Rt lt
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
Reflexes
R L
B + +
T + +
S + +
K + +
A + +
P + +
P/A: SOFT, NON TENDER
I/O:1800ml/800ml
GRBS: 108MG/DL
A
Altered sensorium secondary to ?sepsis ? TB meningitis
?AKI ( Pre renal)
?Cor pulmonale
? B/L pulmonary koch's with iron deficiency anemia
P
1. IV FLUIDS NS @ 75 ml/hr
2. RT feed
200 ml water 2 nd hrly
200 ml milk 4th hrly
3. Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
Mucomist - 4 th hrly
4.SYP.GRILLINCTUS - 15 ml RT/TID
5.CPAP - Intermittently
6.Oxygen support to maintain spo2 88-94%
7.GRBS - 7 POINT PROFILE
8.Vitals monitoring 2nd hrly.
1/5/23
S
Stools passed
No fever
O
Pt is conscious, Not coherent to time,place, person and irritable
Speech is normal
No meningeal signs
GCS E 4 V4 M5
BP - 120/80 mm hg
PR - 84 bpm
SPO2: 92% ON RA
RR: 24 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ ,WHEEZE(Expiratory) +
Rt lt
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
Reflexes
R L
B + +
T + +
S + +
K + +
A + +
P + +
P/A: SOFT, NON TENDER
I/O:2400ml/1050ml
GRBS: 124MG/DL
A
Altered sensorium secondary to ? Pyogenic meningitis ? TB meningitis With AKI (pre renal) resolving
?Cor pulmonale with COPD( emphysematous)
? B/L pulmonary koch's with iron deficiency anemia
P
1. IV FLUIDS NS @ 75 ml/hr
2. RT feed
200 ml water 2 nd hrly
200 ml milk 4th hrly
3. Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
Mucomist - 4 th hrly
4.SYP.GRILLINCTUS - 15 ml RT/TID
5.CPAP - Intermittently
6.Oxygen support to maintain spo2 88-94%
7.GRBS - 7 POINT PROFILE
8.Vitals monitoring 2nd hrly.
2/5/23
S
No fever spikes
O
Pt is conscious, Coherent to person, Not coherent to time,place and irritable
Speech is normal
No meningeal signs
GCS E 4 V4 M6
BP - 130/70 mm hg
PR - 74 bpm
SPO2: 91% ON RA
RR: 22 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , B/L WHEEZE + R>L
Rt lt
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
Reflexes
R L
B + +
T + +
S + +
K + +
A + +
P + +
P/A: SOFT, NON TENDER
I/O:2400ml/1400ml
GRBS: 131MG/DL
A
Altered sensorium secondary to ? TB meningitis ? Pyogenic meningitis with AKI (pre renal) resolved with
? COPD( emphysematous)
? B/L pulmonary koch's with iron deficiency anemia
P
1. IV FLUIDS NS @ 75 ml/hr
2. RT feed
200 ml water 2 nd hrly
200 ml milk 4th hrly
3.Inj.MONOCEF 2g IV/BD
3. Inj.LASIX 40mg iv /OD 4.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
Mucomist - 4 th hrly
5.SYP.GRILINCTUS - 15 ml RT/TID
6.CPAP - Intermittently
7.Oxygen support to maintain spo2 88-92%
8.GRBS - 6th hrly.
9.Vitals monitoring 2nd hrly.
10.Tab.RIFAMPICIN 150mg
Tab.ISONIAZID 75MG
Tab.PYRIZINAMIDE 400MG
Tab.ETHAMBUTOL 275MG
11.Tab.PYRIDOXINE 50MG PO/OD
3/5/23
S
No fever spikes
O
Pt is conscious, Coherent to time and person, Not coherent to place and slightly irritable
GCS E 4 V5 M6
BP - 120/80 mm hg
PR - 92 bpm
SPO2: 91% ON RA
RR: 22 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , Rt. IAA,ICA,IMA Expiratory rhonchi present
Rt lt
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
Reflexes
R L
B + +
T + +
S + +
K + +
A + +
P + +
P/A: SOFT, NON TENDER
I/O:2900ml/1750ml
GRBS: 112MG/DL
A
Altered sensorium secondary to ? TB meningitis ? Pyogenic meningitis with AKI (pre renal) resolved with
COPD( emphysematous)
B/L pulmonary koch's with iron deficiency anemia
P
1. IV FLUIDS NS @ 75 ml/hr
2. RT feed
200 ml water 2 nd hrly
200 ml milk 4th hrly
3.Inj.MONOCEF 2g IV/BD
4. Inj.LASIX 40mg iv /OD
5.Tab.RIFAMPICIN 150mg
Tab.ISONIAZID 75MG
Tab.PYRIZINAMIDE 400MG
Tab.ETHAMBUTOL 275MG
6.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
Mucomist - 4 th hrly
7.Oxygen support to maintain spo2 88-92%
8.GRBS - 6th hrly.
9.Tab.PYRIDOXINE 50MG PO/OD
10.Vitals monitoring 2nd hrly.
11.Chest physiotherapy
ATT started from 2/5/23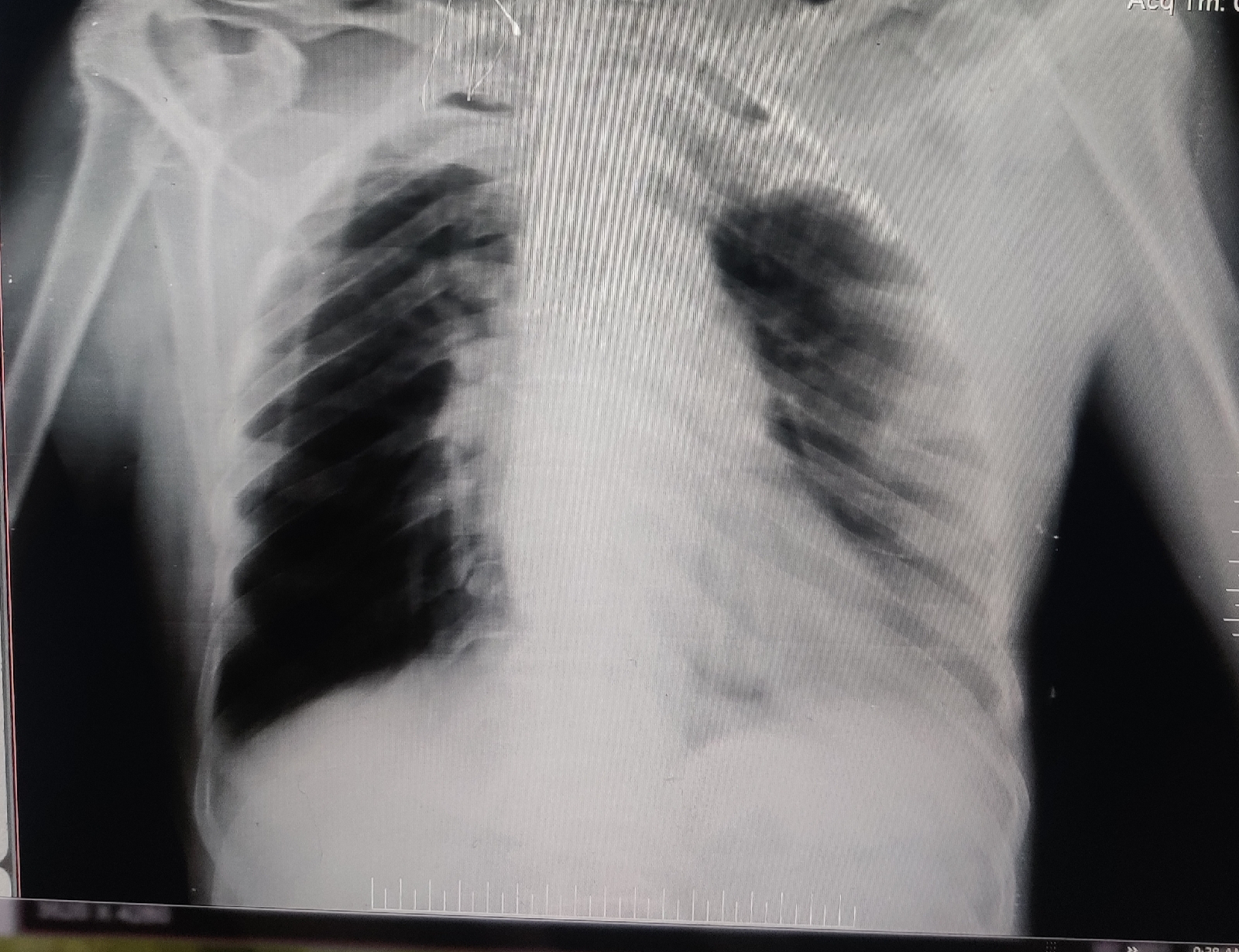























Comments
Post a Comment